Provo’s Eye Center for Keratoconus Treatment
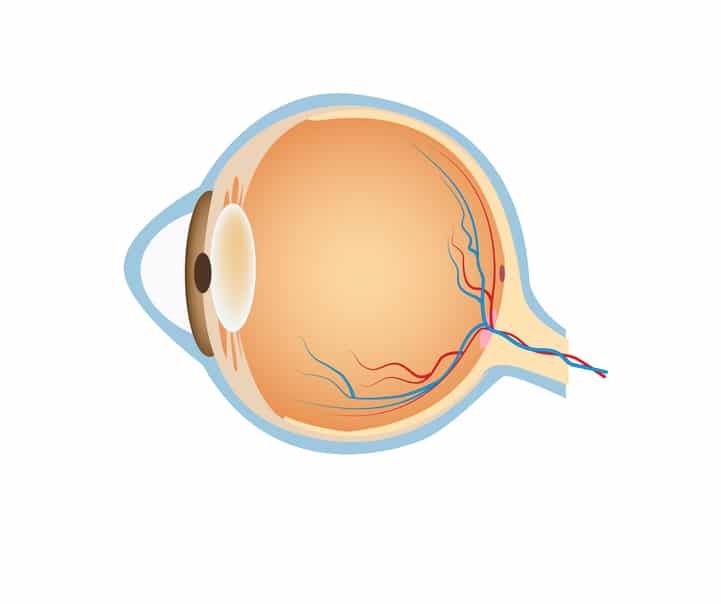
Keratoconus (ker-uh-toe-KOH-nus) occurs when your cornea—the clear, dome-shaped front surface of your eye—thins and gradually bulges outward into a cone shape. Often patients do not know they have keratoconus and have been told that their eyes simply can’t see 20/20, causing them to give up on trying to achieve better vision. However, there are signs and solutions for this condition, and our team is here to provide support.
This condition is known to cause astigmatism and nearsightedness, which may require frequent changes to your corrective lens prescription. If your vision worsens year after year, contact our team for a comprehensive eye exam. We can help you explore various treatment options to manage keratoconus and other sight conditions effectively.
How We Diagnose Keratoconus
Keratoconus is diagnosed during an eye exam by using a microscope to look directly at the cornea, using a corneal topographer to map the cone shape, and using pachymetry to measure the thickness of the cornea.
With keratoconus, a cone-shaped cornea causes blurred vision and may cause sensitivity to light and glare. Keratoconus usually affects both eyes, though it often affects one eye more than the other. It generally begins to affect people between the ages of 15 and 25. The condition may progress slowly for 15 years or longer.
Early Keratoconus Symptoms
How Do You Treat Keratoconus?
Mild keratoconus may be treated with glasses or soft contact lenses. Moderate to advanced keratoconus is typically treated with rigid gas permeable lenses (RGP) or large rigid contact lenses called scleral lenses. Some patients with keratoconus require corneal surgery for intacs implants or corneal transplants. With today’s contact lens technology, we can usually avoid corneal surgery.
In 2016, the FDA approved a minimally invasive procedure called corneal cross-linking to minimize the progression of keratoconus. During this procedure, a doctor will instill a medicated eye drop and then expose the cornea to ultraviolet (UV) light from a special instrument to strengthen the tissues of the cornea. The goal is to keep the cornea from bulging more. It’s called “cross-linking” because it adds bonds between the collagen fibers in your cornea. They work like support beams to help the cornea remain stable.

Provo’s Keratoconus FAQs
Pachymetry or corneal pachymetry is a test that measures the thickness of the cornea using a specialized device called a pachymeter. This test is essential for optometry professionals to assess conditions like keratoconus or to determine the suitability of a patient for refractive surgery based on corneal thickness measurements.
Scleral lenses are custom-fit to help patients achieve dramatic improvements in visual acuity and comfort. Scleral lenses vault over the cornea and prevent discomfort by resting on the sclera so as not to place any pressure on the irregular cornea. This creates a new optical surface to replace the distorted cornea caused by keratoconus.
While there is no definitive way to prevent keratoconus, individuals can take steps to reduce their risk factors.
For those with a family history of the condition or certain systemic disorders linked to keratoconus, regular eye exams can help monitor for early signs of the disease.
To lower the risk of chronic eye inflammation contributing to keratoconus, it is essential to manage allergies and avoid irritants that may worsen inflammation. Additionally, avoiding chronic eye rubbing and seeking treatment for underlying eye conditions can help decrease the risk of developing or worsening keratoconus.
Regular eye care and early intervention can play a crucial role in managing keratoconus risk factors and maintaining overall eye health.
Request an Appointment
Take control of your vision today. Regular eye exams and taking steps to reduce eye irritation and inflammation can help manage the risk factors associated with keratoconus development.
If you have less than optimal vision, suspect you have keratoconus, or know you have keratoconus, call us today to schedule an evaluation. During the exam, we will map your cornea for a definitive diagnosis. We will map your cornea yearly to monitor the progression of this very treatable disease. Call (801) 373-4550 or request an appointment using the link below.
